FRED DE SAM LAZARO, NewsHour correspondent: In the forests along Cambodia’s border with Thailand, scientists have spotted early signs of drug-resistant malaria that could threaten millions of lives far beyond these isolated villages. But their first challenge is finding patients.
It took nearly two hours for a team from the regional center in Thasanh to reach the village of Samlot, which has seen several dozen malaria cases in recent weeks.
“Is anyone you know ill,” they asked? A short walk down the road took them to 22-year-old Pin Sreymom. She was too weak to work the family’s small farm field.
DOCTOR (through translator): Have you been vomiting?
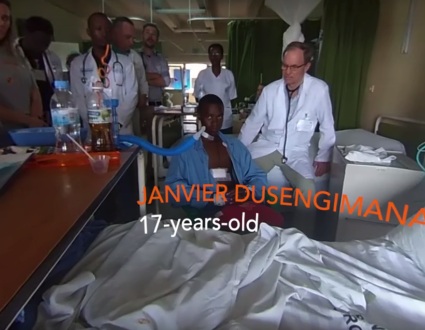
FRED DE SAM LAZARO: But inside their tiny home, her 19-year-old brother, Pin Vantim, was in even tougher shape, with a searing temperature that, along with nausea and vomiting, are malaria symptoms. Both siblings agreed to be tested to confirm the diagnosis before they got any treatment. Until now, Pin Vantim had refused all help.
PIN SREYMOM (through translator): Even if you give him pills like paracetamol, if you’re not paying attention, he’ll throw them out.
FRED DE SAM LAZARO: He even refused to get free treatment available at the health center because he’s afraid of both pills and needles. His sister didn’t go because it costs too much to get there, and she didn’t want to leave the house unguarded. There are lots of reasons people don’t take advantage of the offer of free care.
PIN SREYMOM (through translator): I don’t want to go. There’s no one to take care of the house. I’m afraid to leave it unattended for so long.
FRED DE SAM LAZARO: So like most people who get ill around here, she got some pills from an aunt who bought them from a nearby store. This is a typical example of how drug resistance can begin: A patient doesn’t follow the prescription and, in this case, takes only a partial dose.
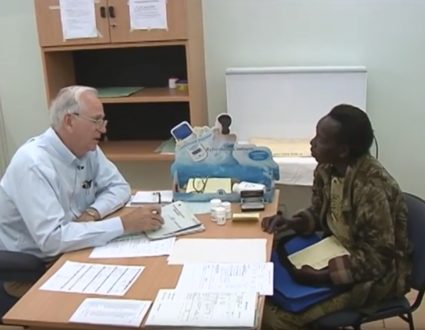
DR. DARAPISETH SEA, Cambodia Ministry of Health: This one will have to take four dose, but this one have only two dose.
FRED DE SAM LAZARO: So she’s taking the right stuff, but not sufficient amounts of it?
DR. DARAPISETH SEA: Not sufficient, yes.
FRED DE SAM LAZARO: Taking less than a full dose means some parasites remain in the body, where they adapt genetically and become immune to the drug. Dr. Darapiseth Sea of Cambodia’s health ministry says many patients are simply too poor to afford the whole dose.
DR. DARAPISETH SEA: They have only enough amount of money to buy only some drug, and then…
FRED DE SAM LAZARO: Not enough for the whole course, in other words?
DR. DARAPISETH SEA: Yes, not enough for the course. And sometimes when they get better, they feel that don’t need more medicine, so they throw the rest away.
FRED DE SAM LAZARO: Or they save it for somebody else, possibly.
DR. DARAPISETH SEA: Sure.
FRED DE SAM LAZARO: Another source of partial-dosing comes in counterfeit drugs, mostly from China and Thailand. They contain only a fraction of the active ingredients, so they can be sold cheaply, sold without prescription, and mostly by people with no training.
There are quality problems even in pharmacies, like this one we stopped by in Battambang, Cambodia’s second-largest city. I asked for malaria medications.
We can see that the expiration date here is May of 2008. So this is an expired drug, but it’s on the shelf.
A customer stopped by complaining of diarrhea. She swallowed one antibiotic pill. There’s no guarantee she’ll return for the rest of what should be a three-pill regimen.
YUN SAMEAN, translator: She just came and took one pill. Maybe they take one time, and then, when she doesn’t feel better, she come back.
Signs of resistance
FRED DE SAM LAZARO: The malaria parasite first became resistant to chloroquine in the ’70s, then mefloquine. Now there are early signs of resistance to the most effective drug currently on the market, artemisinin, or artesunate.
LT. COL. MARK FUKUDA, U.S. Army: So one of the things we have to think about is what our next study is going to be here.
FRED DE SAM LAZARO: Dr. Mark Fukuda co-authored one study with such findings. He’s with the U.S. Army, one of several international agencies working on a renewed effort to contain the problem here.
It’s sponsored largely by the Bill and Melinda Gates Foundation. The foundation is also an underwriter of the NewsHour.
LT. COL. MARK FUKUDA: In very few instances, those parasites do appear to return, and they appear to return despite the fact that there are adequate blood levels of an anti-malarial in their blood. In this case, the concern is, is that the — the resistance is occurring to the — the last widespread anti-malarial available for use, and that is artesunate.
FRED DE SAM LAZARO: There’s no backup drug if this one fails, in other words?
LT. COL. MARK FUKUDA: There are drugs in development at the moment, but there’s no backup that’s readily accessible at this point.
FRED DE SAM LAZARO: The stakes are high in Cambodia, where about 200 people died from malaria last year. But they are huge in Africa, where thousands of mostly children die every day. The history with previous malarial drugs that became ineffective is a disturbing guide, says Fukuda.
LT. COL. MARK FUKUDA: The resistance originated in Southeast Asia and spread to sub-Saharan Africa. That happened, and it’s been documented with scientific studies, contemporary studies, with chloroquine, as well as Fansidar. And if that pattern holds true — and there’s no reason to expect it wouldn’t, because of global travel today — that that’s the pattern, that’s the concern of spread. And so, hence, there’s this effort on trying to contain parasites.
FRED DE SAM LAZARO: The effort includes distributing bed nets to keep out mosquitoes, which spread malaria to humans, and stepping up screening. But most importantly, the scientists want to limit the parasite’s exposure to artesunate to preserve its effectiveness.
So Cambodia’s government has banned its use as a solo drug. It’s allowed only in extreme cases in health centers. All others have to use a blend of artesunate and older drugs that are no longer as effective by themselves, but work in combinations.
LT. COL. MARK FUKUDA: The thing about this is it could be, if it’s legitimate, it’s a good treatment, but it’s not a government — it’s not part of the national regimen, so it’s an example of how private sector outlets are unregulated. It could be good; it could be bad.
FRED DE SAM LAZARO: So you just don’t know whether this is the real article or something…
LT. COL. MARK FUKUDA: Right.
Cracking down on illegal sources
FRED DE SAM LAZARO: However, given the remote border region, the lack of much law enforcement, there’s no guarantee artesunate it won’t come in from illegal sources. Michael O’Leary heads the World Health Organization’s Cambodia office.
MICHAEL O’LEARY, M.D., World Health Organization: What manufacturers, what some illicit manufacturers will do then is put a small amount of the active drug in their product so that it can, in fact, pass simple tests and so on and also have some effect and sell those at substantial profit.
So there’s a lot of stimulus to do that. There has been an effort with international policing agencies, with health agencies, and so on, to clamp down on this, on this flow of drugs across the border, and that’s one way that has been at least moderately effective.
FRED DE SAM LAZARO: Later this year, in a European-sponsored program, international agencies here hope to take a different tack against the illicit medicines, a price war to run the counterfeiters out of business.
MICHAEL O’LEARY: We have a new mechanism which would put heavily subsidized malaria drugs on the market and allow them to be sold at very low prices, a fraction of what they’re currently being sold for, and therefore flood, as you say, the market with high-quality drugs, at low prices, that can actually undercut the illegal drug trade.
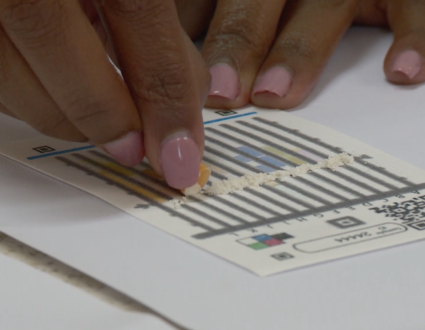
FRED DE SAM LAZARO: The plan also calls for training local village volunteers to diagnose malaria cases, utilizing rapid test kits that are now available.
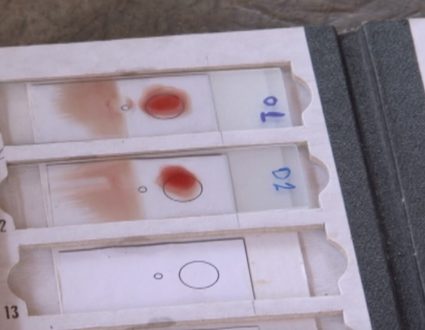
So it takes a little — a pinprick.
DOCTOR: Drop of blood.
FRED DE SAM LAZARO: Drop of blood.
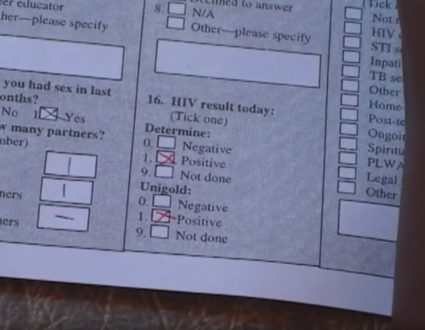
DOCTOR: And then you put a — there’s a solution you put here into the blood. It then migrates here. You can imagine it’s simple, like a pregnancy test kit.
FRED DE SAM LAZARO: Some kits in local hands would ensure that patients like Pin Sreymom and Pin Vantim are reached far sooner.
DOCTOR (through translator): Make sure to take all the pills we have given you.
FRED DE SAM LAZARO: As the team suspected, there was a lot of the deadly malaria parasite in Pin Vantim’s blood. His sister, because she took some medicine, had a lower level of infection.
Dr. Darapiseth urged her to take all her pills, then issued a dire warning about her brother.
DR. DARAPISETH SEA (through translator): If you can, you must take him to the hospital. Do not worry about the money. If he doesn’t get treatment, he’s going to die. I don’t want to scare you, but that’s the truth. If you didn’t take the pills, you would have been just like him.
FRED DE SAM LAZARO: The stern talk was enough to coax him to take at least the first of the four doses in the combination therapy. For the team, it was one tiny step in a very long journey to contain drug-resistant malaria and a much longer one to eradicate it.
Hunting the Strain
Drug-resistant malaria is threatening villages in western Cambodia. NewsHour special correspondent Fred de Sam Lazaro reports from the border region of Cambodia and Thailand.